Basics of Surgical Oncology - Juniper Publishers
Cancer Therapy & Oncology - Juniper Publishers
Abstract
This article aims to standardize terms used in
Surgical Oncology that are the basis for the treatment of cancer
patients. Terms like: Patient out of cancer treatment, Patient in stage
IV, In block tumor resection, Ganglionic relay, Local and regional
control, Systemic Control, Unknown Primary Origin, Unresectability,
Inoperability, Multiple Organ Resection, Preoperative Nutritional
Status, Minimum Oncologic Procedure, Resection margins, Prognostic
Factors, Peritoneal Washing Cytology, Adjuvant, Neoadjuvant and
Peri-adjuvant Therapy.
Keywords: Basic terms in Surgical Oncology; Cancer Surgery
Abbreviations: OCT: Patient Out of Cancer Treatment; UPO: Unknown Primary Origin; BMI: Body Mass Index.
Introduction
There are basic oncological principles universally
accepted and those principles were born from the experience accumulated
in Cancer Treatment Centers after years of observing the results
obtained in large series of patients undergoing various treatment
protocols both medical and surgical. We will define these concepts or
basic criteria that should be on the minds of all physicians who manage
patients with cancer. To address the issue we will split the patients
into two groups: OCT patients and patients admitted for treatment.
Patient out of cancer treatment (OCT)
A patient is OCT when IS NOT A CANDIDATE for treatment except palliation. This is accomplished with the following criteria:
Patient in stage IV not requiring palliative surgery:Patients that should be excluded from this category are:
Unknown Primary Origin:Since in this case the patient may have a neoplasm that may be treatable (such as lymphoma).
Lymphoma, myeloma or leukemia:These patients can be offered node biopsy or bone marrow studies and treatment with chemotherapy or radiotherapy.
Choriocarcinoma and Gestational Trophoblastic Disease:These tumors are very sensitive to Methotrexate.
Ovarian Cancers:These patients are candidates to Cytoreductive Surgery and Chemotherapy.
Seminoma and testicular tumors:Patients that are also candidates to cytoreductive surgery and radiotherapy.
Breast cancer:Advanced stage may be treated with chemotherapy and radiotherapy.
Prostate cancer:These are radiosensitive tumors.
Palliation should only be done when the patient himself requests it.
Gallbladder and bile duct Cancers CAN NOT BE TREATED WITH SURGERY. Those are best palliated with computerized brachytherapy.
Multiple studies have shown that a temporary
palliation can be achieved with ultrasound-guided percutaneous drainage.
But currently the best palliative treatment for these cancers is
computerized brachytherapy. Gallbladder cancer in an early stage is
curable with cholecystectomy alone. Advanced stages do not improve their
prognosis with surgical resection (segmentectomy of IV segment,
lobectomy). Surgery has proven to be counterproductive (it shortens
survival and impairs the patient’s quality of life). Patients with
gallbladder and bile duct cancer (intra or extrahepatic) are not
admitted for surgical treatment as they are inoperable, they cannot
receive Chemotherapy (tumor is not chemosensitive), neither radiotherapy
(liver tissue is too sensitive to radiation and it will damage the
liver before it hits the tumor). The only suitable treatment is
computerized brachytherapy.
A Patient is in Stage IV When
- There is ganglionic invasion beyond a certain node relay.
- There are lung metastases (circular images in X-rays).
- There are liver metastases (demonstrated by ultrasonography or elevated transaminases).
- There are bone metastases (in X-ray series and bone alkaline phosphatase elevation).
- There are brain metastases (CT Scan).
It is important to first do all these determinations to decide
whether or not a patient is in stage IV.
Patient Admitted for Cancer Treatment
Before deciding on the type of surgery and the purpose of it
(palliative, diagnostic or curative) is necessary to consider each of the following concepts.
In Block Tumor Resection
It is when a tumor is removed in continuity with its
ganglionar nodes in a single block. This is the ideal in Oncology
because if the tumor is removed and the ganglionar tissue is
removed apart, the lymph paths between the nodes and the
tumor will be open and we will be spreading the tumor. It may
not always be possible to do so, but if the tumor is in continuity
with the corresponding relay node, an In block resection must
be planned.
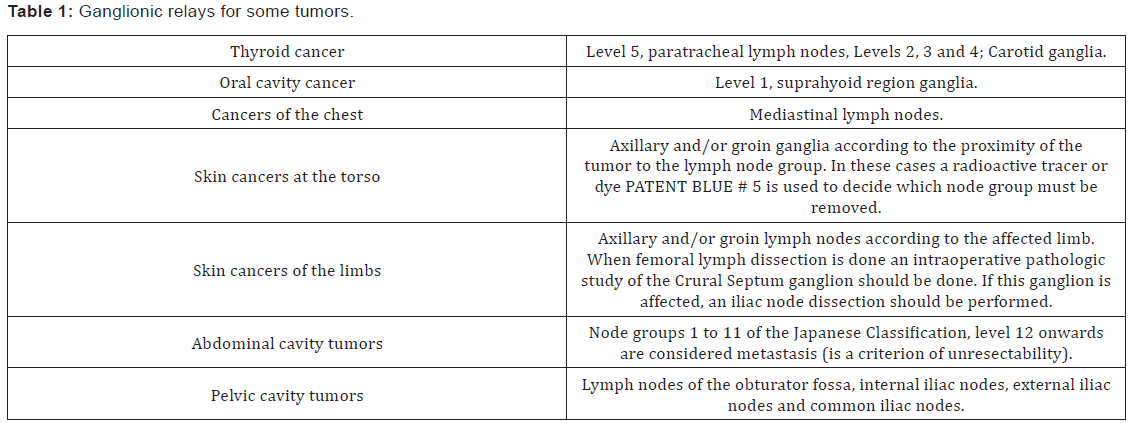
First Lymph Node Relay
In cancers with lymphatic spread a group of nodes is
established for each tumor that are the gateway for producing
metastasis. A better local and regional control of the disease is
achieved if this group of nodes is removed. Ganglionic relays for
some tumors are (Table 1):
Local and regional control.
No radical surgery can achieve a Cancer Systemic Control. It
has been established that there is no surgical procedure in any
type of tumor (except carcinoma in situ in some cases) which
can guarantee that no tumor cells have been left in the patient.
The surgeon can only remove the tumor and the first lymph
node levels. In gastric cancer Japanese have proposed extensive
resections but no significant advantages have been found. In
breast cancer the three nodal levels can be removed and in neck
cancers a radical dissection can be performed but even in these
cases the surgeon is only cleaning the first node levels. The only
way to achieve a Cancer Systemic Control is with chemotherapy,
radiation and/or hormone therapy. So in general a patient
should be referred to the Medical Oncologist.
In some cancers, radiation therapy has replaced surgery
as it has been shown to achieve the local and regional control
equally or even better than surgery, because surgery sometimes
is mutilating. In Oral Cavity and Pharynx Cancers Radiotherapy is better than surgery for stages I-II. Also Radiotherapy is
better than Surgery for Cervical Uterine Cancer stage IIB. When
operating a patient with Uterine Cervical Cancer one should
keep in mind that if we find parametrial induration the Surgery
should be suspended, and the patient should be referred for
Radiation Therapy. We would only increase the morbidity of
these patients if we perform a hysterectomy.
Unknown primary origin (UPO)
In this term there is a discrepancy in the literature but
I consider it is more practical to define it as a stage IV cancer
in which it was not possible to identify the primary origin.
These patients are examined because a treatable tumor can be
found, especially when the biopsy reports an undifferentiated
tumor (that usually is really a lymphoma). In these patients a
laparoscopic retroperitoneal lymph node biopsy is performed if
needed for diagnosis. In such cases the purpose of surgery is to
make diagnosis or palliation, not a curative surgery.
Unresectability
It is considered that a tumor is unresectable if it is in an
advanced stage and the tumor cannot be removed, even if a
radical surgery is performed. This occurs in stage IV tumors or in
cases of Carcinomatosis. Unresectability does not contraindicate
surgery and can be done with palliative or diagnostic purposes.
Inoperability
It is when the patient’s physical condition has a prohibitive
surgical risk, such as in elderly patients with heart, renal,
respiratory or liver failure, etc. Inoperability in some patients
can be treated and the patient becomes suitable for surgery.
Multiorgan resection
It is defined when a radical resection may affect three or
more organs. This is an Inoperability criterion. This is a treatable
condition because in some tumors preoperative chemotherapy
or radiotherapy can reduce tumor volume and thus make it
operable.
Nutritional status
Allows evaluating the patient’s condition to tolerate the
post-surgical metabolism. It is very important to determine the
nutritional status in every patient that will be subjected to any
type of surgery, especially in cancer patients because tumors
producing catabolism is something very common. This ideally
should be determined by the nutritionist. But when you do not
have an expert in this field the surgeon can make a fairly accurate estimate with the following parameters:
BMI or Body Mass Index:It is determined by dividing
weight in kilograms by the square of height in meters. An index
that is less than 20 is an inoperability criteria.
Serum Albumin:A serum albumin value lower than 2 g/dl
is an inoperability criteria.
Total lymphocyte count:This value is obtained by
multiplying the percentage of lymphocytes by the total
leukocytes (white blood cell count). A value less than 1000 total
lymphocytes is an inoperability criteria.
There are more parameters to determine the nutritional
status but with only these three that are accessible in almost
all hospitals the surgeon can justify the patient’s condition
for surgery. When the nutritional status of a patient indicates
inoperability criteria, the patient must be submitted to a
supplementary diet until the total number of lymphocytes and
serum albumin levels are correct, which usually requires a
dietary supplement (like Ensure 1 can 3 times a day) and a high
calorie and a high protein diet for a period of at least 15 days.
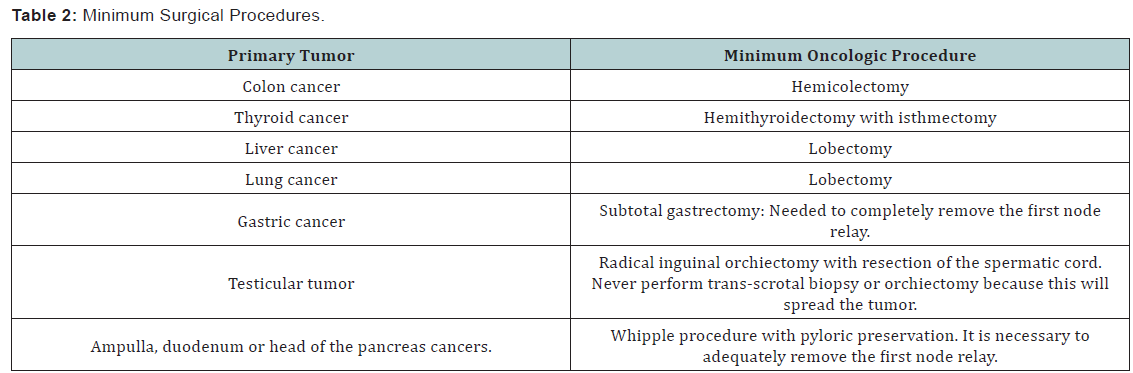
Minimum Oncological procedure
The minimum surgical procedures are already defined in the
literature. These are to be performed for certain types of tumors
and are the minimal tumor resection for an oncologically valid
surgery (Table 2).
Resection margins
Is the distance in centimeters left between the edge of the
tumor and the cut made to remove it. To avoid the risk of leaving
tumor cells the surgeon should always remove a certain amount
of healthy tissue around the tumor. This amount of healthy
tissue is measured in centimeters and in the literature is already
determined how many centimeters away from the edge of the
tumor are necessary. This should be measured in the surgical
specimen during the operation by the pathologist to see if it is
necessary to expand the resection. In general most tumors need a resection margin of at least 2 cm for a proper oncological
resection but some tumors need a wider resection margin.
Adverse prognostic factors.
These serve to establish the prognosis of a cancer patient and
therefore the need for surgery. These are not the “Risk factors”.
A Risk factor is a history of factors that increases the chances of
having a cancer, such as: smoking for lung cancer, contraceptives
for breast cancer, etc. Adverse prognostic factors are those that
determine the probability of death at 1 and 5 years in a patient
who has been diagnosed with cancer. These vary according to the type of tumor and usually these are determined by the
pathological study of a biopsy or a surgical specimen.
The stage of the tumor.The TNM classification is universal.
As a rule all tumors having ganglionic invasion beyond the
first relay node or tumors that invade the muscle layer or the
serous membrane have a poor prognosis. There is data available
to determine the probability of death at 1 and 5 years for each
tumor. It has been established that a surgical procedure is
justified when the probability of survival at 1 year is greater or
equal to 15% (or mortality at one year is less than 85%).
The degree of differentiation.Grade II or III (moderately
differentiated and poorly differentiated tumors) is a factor of
poor prognosis.
The pattern of spread.Well defined tumor edges have
a better prognosis than infiltrating edges. “Fingerlike” or
“raindrops” pattern of spread have a poor prognosis.
Tumor volume.This can be measured in the CT Scan
(ask the radiologist). Except in epithelial ovarian cancer and
choriocarcinoma it has been observed that a tumor volume close
to 1 kg is incompatible with life.
Peritoneal Lavage Cytology
This is a mandatory procedure in surgery of any tumor that
is within the abdominal cavity. It consists of instilling 100 cc
of Sterile Saline Solution in the abdominal cavity and then 50
cc should be recovered. During the operation this sample is
sent to be studied by the pathologist. If the pathologist reports
neoplastic cells in the peritoneal lavage this is a criterion of
unresectability and the surgical procedure should be interrupted
if it is not for palliation purposes. In this case it is not convenient
to realize an extensive surgery because all tissue cleavage sites
release growth factors and trophic factors that accelerate the
implantation of tumor cells and thus the spread of the tumor,
and the patient survival will be shortened. Other protocols use
in addition multiple biopsies including: biopsy of para-aortic nodes, biopsy of parietal peritoneum, spleen and liver biopsy
to determine if there is tumor spread before performing the
surgical procedure.
Adjuvant, neoadjuvant and peri-adjuvant
In several types of cancers is necessary to apply
Chemoradiotherapy before surgery or after. Before surgery
(neoadjuvant therapy) reduces the tumor stage and increases the
likelihood that the resection margins will be negative to tumor
cells. Also we must remember that no radical surgery can achieve
Systemic cancer control. For example, in rectal cancer it is already
accepted worldwide that preoperative Chemoradiotherapy
increases the likelihood of a curative resective surgery. In some
tumors where the neoadjuvant Chemoradiotherapy is not used
a subsequent systemic treatment (adjuvant therapy) within 6
to 8 weeks after the surgery it is recommended. Peri-adjuvant
is when you apply Chemoradiotherapy before and after surgery
[1-5].
Conclusion
It is important to standardize the basics of Surgical Oncology.
To Know more about Cancer Therapy & Oncology
Click here: https://juniperpublishers.com/ctoij/index.php
click here: https://juniperpublishers.com/



Comments
Post a Comment