Juniper Publishers - The Effect of Different Single Doses from X-Rays on Pediatrics Rhabdomyosarcoma Tumor Cells: In Vitro Survival Curve
Cancer Therapy & Oncology International Journal
Abstract
The purpose of the work was to study the effect of different single radiation doses of X-rays on the pediatrics Rhabdomyosarcoma (RMS) cells in vitro. In addition, to construct the survival curve for the RMS cells and determine some crucial radiobiological parameters used for calculations of tumor cell kill in radiotherapy treatment of pediatrics RMS tumors.
An established in vitro cell culture model employing the RMS tumor cell lines was used for this study. Cells were exposed to single doses of 0, 4, 8, 12, 16, and 20 Gy from a 6 MV X-rays photon beam energy. The clonogenic cell survival assay method was used to quantify the RMS cell survival. The survival curve was fitted by the single-hit multi-target and linear-quadratic models.
The mean lethal dose (D0=3.2 Gy), the extrapolated number (n=11) represents a measure of the width of the survival curve shoulder and corresponds to the number of sub-lethal targets, and the dose at which the contributions of linear and quadratic components of cell killing are equally (α⁄β=9 Gy) were determined for the RMS cells.
The survival curve parameters for the RMS cells were determined. Low radiosensitivity of cells under study in vitro was concluded. Conventional dose of 2 Gy per fraction should provide therapeutic gain with an increased tumor control probability (TCP) and decreased normal tissue complication probability (NTCP) for radiotherapy treatment.
Keywords: Cell Survival Curve; Rhabdomyosarcoma; In Vitro Cell Culture; Linear-Quadratic Model; Single-Hit Multi-Target Model; Radiobiology
Abbreviations: TCP: Tumor Control Probability; NTCP: Normal Tissue Complication Probability; SF: Surviving Fraction; ROCS: Radiation Oncology Computer System; SSD: Source to Surface Distance; RMS: Rhabdo Myo Sarcoma; PBS: Phosphate Buffered Saline; BSC: Bio Safety Cabinet; ATCC: American Type Culture Collection
Introduction
Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma of childhood. RMS tumor exhibits the skeletal muscle differentiation [1,2]. The two major histiotypes, embryonal and alveolar, are characterized by specific genetic abnormalities that provide clues to the mechanisms of tumor induction [1]. Contemporary risk-based therapy cures more than two thirds of children with RMS while minimizing acute and late effects [1]. To examine the capability of a group of single cells to grow and form colonies after being irradiated to different single radiation doses, reproductive integrity measure is a convenient proof that the cells retained their functions. The loss of this ability as a function of radiation dose is described by the dose-survival curve. A cell survival curve describes the relationship between the radiation absorbed dose and the proportion of cells that survive (or surviving fraction) [3,4]. For a tumor to be eradicated in a single fraction in radiotherapy, it is only necessary that cells be killed in the sense that they are rendered unable to divide and cause further growth and spread of the malignancy [3].
The radiation survival curve was demonstrated by Puck and Marcus [5] for cultured HeLa cells exposed to X-rays. Since then it has remained the basic method used in quantitative radiobiology. Several research works [6-13] were conducted on the survival curve parameters for different normal and malignant cell organisms, including bone marrow stem cells, cartilage, epithelial cells, intestinal mucosa, parenchyma hepatocytes, hyperthermia, lung, skin colonies, skin fibroblast,mammary cells, etc. both in vitro and in vivo. The purpose of the work was to study the effect of different single radiation doses from X-rays on the pediatrics Rhabdomyosarcoma (RMS) cells in vitro. In addition, to construct the survival curve for the RMS cells and determine some cruciall radiobiological parameters used for calculations of tumor cell kill in radiotherapy treatment of pediatrics RMS tumors.
Materials and Methods
Cell Lines and Sample preparation
Human Rhabdomyosarcoma (RMS) cells were obtained from ATCC (American Type Culture Collection, Manassas). An established in vitro cell culture model employing the RMS tumor cell lines at the National Health Laboratory was used in this study following the World Health Organization guidelines [14,15]. The RMS cells as a confluent monolayer in a culture flask were maintained in growth medium supplemented with 10% fetal calf serum. Growth medium from the cell culture flask was decanted and the confluent cell layers were washed twice with Ca and Mg free phosphate buffered saline (PBS) in bio safety cabinet (BSC). A 0.25% trypsin reagent solution was added to the monolayer. The flask was kept in a 36°C incubator until the cells detached from the surface. Complete detachment of cells was checked with the inverted microscope device. The cells were re-suspended in the growth medium, and the desired concentration was adjusted to 1600 cells/ml in 15 capped cell culture tubes (Figure 1). RMS cells in culture tubes were left in an incubator at 36°C condition for 1 hour before the irradiation.
Radiation Therapy and Sample Irradiation
RMS cells in the culture tube were exposed to 0, 4, 8, 12, 16, and 20 Gyradiation doseswith a therapeutic X-ray linear accelerator machine (Elekta 75/15, with 6 MV photon beam energy and 600 MU/min dose rate) at Radiation and Isotopes Center – Khartoum. The irradiation was performed with a source to surface distance (SSD) set up with 100 cm SSD (parallel opposed beams). Two layers of water equivalent bolus (2 cm thick) were used to fit the culture tubes in addition to get rid of air cavities. The dose calculations were performed on Radiation Oncology Computer System (ROCS) version 1.5.6.
Clonogenic Survival
The irradiated culture tubes contain the RMS cells were sub-cultured for a period of 5 to 7 days. The culture tubes with RMS cells were incubated in an incubator maintained at 36°C temperature condition supplied with CO2 from the cell metabolism and 7.2 pH included in basal growth media. The RMS cells were left to divide and grow until the surviving cells form macroscopic colonies. The clonogenic cell survival assay method was used to quantify the cell survival. The colonies formed by the survived cells after the irradiation were calculated using haemocytometer chamber or cells counting chamber based on Freshney (improved Neubauer type). The cell culture tubes with the RMS cells were mixed well with a fine Pasteur pipette in a mixer (Denley Spiramix) and a sufficient volume was aspirated to fill both sides of the haemocytometer chamber slides. The visible formed colonies were counted. The plating efficiency of the RMS cell culture (PE), the percentage ratio of the number of colonies observed to the number of cells plated, was calculated for the control cells [3]. The surviving fraction (SF) of the treated RMS cells, the percentage of the number of colonies counted to the number of cells seeded normalized to the plating efficiency of the control cells, was calculated for each dose [3].
Mathematical Models for Survival Curve description
Various mathematical functions have been used to represent the survival curves. These models are intended to provide values of the surviving function while agree with the experimental values over the range of doses studied, allowing for their statistical precision. In this work, single-hit multi-target and linear-quadratic models [3,16] were used for the description of the survival curve. Single-hit multi-target model assumes that the cells contain n distinct and identical targets which can be individually inactivated by the passage of a charged particle. Inactivation of a target represents a sub-lethal event and the cell is killed when all n targets have been inactivated. The surviving fraction (or survival, S) of cells corresponding to this type of lethality is given by this equation [1]
Where S is the fraction of cells survived after being exposed to a dose D. D0 Is the mean lethal dose for which the mean number of lethal events per cell is equal to one (or for a dose D0 there is on average one hit per target). n is the extrapolated number and it corresponds to the number of sub-lethal targets.
The linear-quadratic model assumes a cell can be killed in two ways, either by a single lethal event or by the accumulation sub-lethal events. If these modes of cell death are taken to be independent, the probability of survival (S) is the product of the probabilities of each type of lethal event [3,16] as given in equation [2]
Where, S is the fraction of cells surviving after a dose D. α is a constant representing the linear component of cell killing. β is a constant representing the quadratic component of cell killing.
Results and Analysis
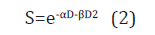
The radiation survival curve for the Rhabdomyosarcoma cells was constructedusing the in vitro cell culture technique. The surviving fraction was plotted on a logarithmic scale versus the absorbed dose on a linear scale. Two mathematical functions depend on the cell target theory models, single-hit multi-target model and linear-quadratic methodical models, recommended for analysis of in vitro radiation data [17] were used for description of the survival curve.
In single-hit multi-target model the surviving fraction and the dose (cGy) results were fitted using equation (1) as shown in (Figure 2). D0, the final slope(mean lethal dose) interpreted as multiple event killing and it is the dose required to reduce the fraction of survivals from 0.1 to 0.037 (Figure 1), was determined from the curve (D0=3.2 Gy). The extrapolation of the final slope D0 back to the y axis yields n, the extrapolation number. The n value describes the width of the shoulder was determined (n=11) for the Rhabdomyosarcoma cells in this study. The value n corresponds to the number of sub-lethal targets.
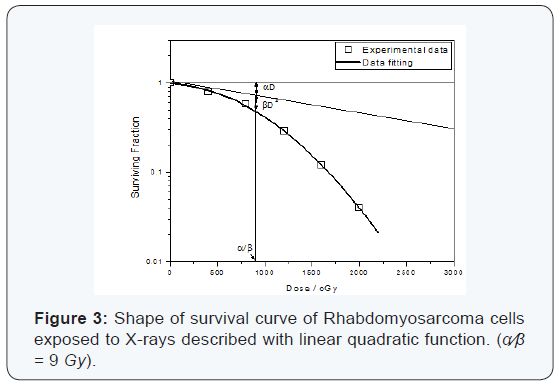
Rhabdomyosarcoma cells exposed to X-rays described by the linear-quadratic function (α⁄β=9 Gy). The curve (Figure 3) shows a tangent at the origin whose slope is -α, followed by progressive downward curvature with increasing dose. The α coefficient is constant describing the initial slope of the cell survival curve, and β coefficient is a smaller constant describing the quadratic component of cell killing. The determined ratio (α⁄β=9 Gy) was the dose at which the contributions of the linear and the quadratic component are equal.
Discussion
For cells growing in culture, the loss of the ability to continue growth is termed reproductive death. Following irradiation, cells may still be intact and able to produce proteins, synthesize new DNA and even go through one or two cell divisions. But if it has lost the capability to reproduce indefinitely, it is considered dead. A survivor that has retained its reproductive integrity and is able to proliferate indefinitely to produce a large clone or colony [3]. When the RMS cells were acutely exposed to X-rays, the ability to divide was declined as a function of radiation dose. The multi-target, one-hit-on-each-target model recommended for analysis of in vitro radiation data [17] seemed adequate for fitting and description the survival curve of the RMS cells exposed to different single doses of X-rays. The model gives rise to survival curves having an exponential form at high doses, and an extrapolation number equal to the assumed number of targets. The mean lethal dose of the RMS cells (D0=3.2 Gy) represents a dose that given an average of one hit per cell. The width of the survival curve, represented by (n=11), indicates that the survival curve for RMS cell type has a broad shoulder (n=10 to 12) [3]. It reflects the ability of the RMS cells to repair sub-lethal radiation damage [18].
A second recommended model for analysis of in vitro radiation data [17] seemed to provide a better fit for our experimental data was the linear-quadratic model. At low doses, the two chromosome breaks are the consequence of a single electron set in motion by the absorption of X-rays. The probability of an interaction between the breaks is proportional to dose (linear portion of the survival curve). At higher doses, the two chromosome breaks may result also from two separate electrons. The probability of an interaction is then proportional to the square of the dose. The survival curve bends if the quadratic component dominates [3]. The α coefficient estimating the intrinsic radiosensitivity, and β coefficient which represents the capacity for repair of sub-lethal DNA damage [3]. The dose at which the linear and quadratic contributions are equal (Figure 2) was determined for the RMS cells (α⁄β=9 Gy). Cells displaying a high α⁄β ratios (α⁄β>6 Gy), they characterized as radioresistant cells and conventional doses per fraction of 2 Gy should provide therapeutic gain with an increased probability of tumor cure and sparing of late-responding normal tissues [18,19]. RMS cells indicate to have low clinical radiosensitivity
Conclusion
Rhabdomyosarcoma tumor cell lines were cultured in vitro. The cells were irradiated to different single doses of X-rays. Clonogenic cell survival assay method was used to quantify the RMS cell survival. The survival curve of the RMS cells was fitted and described using the single-hit multi-target model and linear quadratic recommended models. The survival curve parameters, mean lethal dose, the extrapolation number corresponds to the number of sub-lethal targets, the α⁄β ratio, were determined. Low radiosensitivity of cells under study in vitro was concluded. Conventional dose of 2 Gy per fraction should provide therapeutic gain with an increased tumor control probability (TCP) and decreased normal tissue complication probability (NTCP) for radiotherapy treatment.
To Know More
About Cancer Therapy &
Oncology International Journal Please click on:
https://juniperpublishers.com/ctoij/index.php
To Know More About
Open Access Journals Please click on:
https://juniperpublishers.com/index.php
To know more about Juniper
Publishers Please click on Juniper Publishers



Comments
Post a Comment